- Home
- Common Shoulder Problems
- Brachial Neuritis
Brachial Neuritis
Written By: Chloe Wilson BSc (Hons) Physiotherapy
Reviewed By: SPE Medical Review Board

Brachial neuritis is a rare condition where there is inflammation of the group of nerves that control the shoulder, arm and hand, collectively known as the brachial plexus.
Brachial neuritis is also known as Brachial Plexopathy, Parsonage Turner Syndrome and Neuralgic Amyotrophy.
It is difficult to diagnose accurately and causes severe shoulder pain followed by weakness. Symptoms of Parsonage Turner Syndrome tend to develop quickly without any obvious cause often starting at night and can be extremely unpleasant.
Here we will look at what happens with brachial neuritis, the different types, what causes it, common symptoms, treatment options, prognosis and recovery process.
What Is Brachial Neuritis?
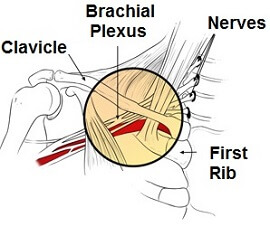
To understand brachial neuritis we need to look at a structure known as the brachial plexus, a collection of nerves found between the neck and the shoulder.
The brachial plexus is a network of intertwined nerves that originate from the root of the neck, pass across the chest over the first rib, through the arm pit (axilla) and down the arm.
It is made up of the lower four cervical nerves (C5-8) and the uppermost thoracic nerve (T1). The brachial plexus controls movement and sensation in the shoulder, arm and hand.
Nerves carry signals from one part of the body for another. They carry messages from the brain telling muscles to contract or relax to produce movement as well as carrying sensory information regarding e.g. touch and temperature. With brachial neuritis, the brachial plexus becomes inflamed and the nerves don’t function normally leading to pain and weakness.
Classification Of Brachial Neuritis
There are two different types of brachial plexopathy:
- Inherited Brachial Neuritis: This is an inherited condition where there is a mutation in the SEPT9 gene on chromosome 17q. It is an autosomal dominant condition. This means that a parent who carries the gene has a 50% chance of passing the faulty gene onto any child they have.
- Idiopathic Brachial Neuritis: This is the most common type. The exact cause is unknown but it is thought to be due to an abnormality in the immune system which causes it to attack the nerve fibres of the brachial plexus resulting in inflammation.
Causes Of Brachial Plexopathy
Brachial neuritis is a rare condition affecting between 1-3 people per 100,000 individuals per year. Whilst the exact cause of Parsonage Turner Syndrome is unknown, possible causes include:
- Infection: Either viral e.g. upper respiratory tract infection or bacterial e.g. pneumonia
- Surgery
- Trauma: injury, not necessarily to the shoulder
- Vaccinations: e.g. ‘flu jab and tetanus
- Child Birth
- Systemic Illness e.g. lymphoma
Symptoms of Parsonage Turner Syndrome
Brachial neuritis symptoms usually come on rapidly, often starting at night. Pain tends to be the first symptom which then gives way to increasing weakness or paralysis.
Common symptoms of Brachial Neuritis include:
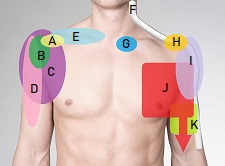
- Sudden, Severe Shoulder Pain: People usually describe it as a sharp, stabbing or burning pain in the shoulder which may spread to the neck, arm and/or hand.
- Pain Worse With Movement: The pain from Parsonage Turner Syndrome usually gets worse with any movement of the arm
- Pain Worse At Night
- Constant Pain: The pain tends to be constant i.e. present every second of every minute of the day, and only eases with strong painkillers
- Affects One Shoulder: It usually only affects one shoulder, most commonly the right, but in some instances can affect both shoulder
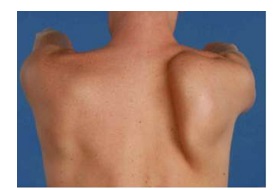
- Shoulder & Arm Weakness: As the pain subsides (this may take days or weeks) muscle weakness/paralysis sets in. The muscle begins to waste, known as atrophy, which is often visible such as a winging scapula making it hard to move the arm. The weakness may be profound, but is usually temporary
- Numbness: If the sensory nerves are affected than your sensation is altered and you may notice some numbness, pins and needles and/or decreased sensation
- Difficulty Breathing: In up to 5% of cases of brachial neuritis the diaphragm is affected which can lead to shortness of breath
- Age Group: Brachial neuritis can affect people at any age (including children which usually indicates the inherited version), but it is most common in young/middle-aged adults
- Gender: Idiopathic brachial neuritis is more prevalent in males, approximately 3:1. Inherited brachial plexopathy affects males and females equally.
Diagnosing Brachial Neuritis
Brachial neuritis can be hard to diagnose and is often misdiagnosed as a neck problem. Your doctor will start by talking to you about your symptoms and will then examine you, looking particularly at your arm movements and muscle strength. They will be looking for signs of muscle atrophy such as scapula winging as shown here. They may also check your reflexes and sensation.
If your doctor suspects Parsonage Turner Syndrome, they will likely send you for imaging studies such as an MRI to rule out other conditions such as cervical radiculopathy and/or shoulder x-ray. Nerve conduction studies or EMG tests looking at the electrical activity of muscles may also be done to see if the nerves are functioning correctly.
This helps to identify whether the weakness is due to a problem in the muscles themselves or a problem with the nerves that control the muscles, the latter of which may indicate brachial neuritis.
Brachial Neuritis Treatment
The initial goal with brachial neuritis is to reduce the pain. Once this has been achieved, you can start on a programme of physical therapy.
#CommissionsEarned from Amazon on qualifying purchases
Treatment for brachial neuritis usually involves:
1. Medication
Pain is usually severe and constant with brachial plexopathy and therefore strong painkillers are often required. These may include narcotic medication (opiates) such as hydrocodone and NSAIDS (non-steroidal anti-inflammatory drugs) e.g. naproxen or ibuprofen/Advil.
Some doctors recommend using corticosteroids such as prednisolone to help reduce inflammation with brachial neuritis, but there is mixed evidence as to the efficacy of this.
2. Physical Therapy
In the early stages of brachial neuritis you will be advised to rest until your pain is under control, but then it is important to start physical therapy to address the associated muscle weakness and loss of movement. The aims of physical therapy are to:
Improve Range of Movement
In the early stages, physical therapy for brachial neuritis will focus on maintaining and improving therange of movement in the shoulder and arm. This will be done through
Passive Exercises: these are when the arm is moved without the muscles having to work, either by someone else moving your arm, or you using your good arm to support the arm and lead the movement.
Active Exercises: Once the pain is under control you can then move to active range of movement exercises (where you perform the movement yourself with the affected arm).
Regain Strength
Once your brachial neuritis pain is under control you can progress to more challenging:
- Rotator Cuff Strengthening Exercises: improve the strength and control around the shoulder
- Scapular Stability Exercises: regain the strength and control around the shoulder blade
Your physical therapist may also use treatments such as ice packs, heat packs and/or TENS machines (transcutaneous electrical nerve stimulation) to help relieve pain.
3. Surgery For Brachial Neuritis
If the symptoms of Parsonage Turner Syndrome fail to settle after a number of months, your doctor may recommend surgery.
This usually consists of nerve grafts and/or tendon transfers, where healthy sections of nerves or tendons are taken from elsewhere in the body and used to repair the damaged nerves/tendons to restore muscle function.
Recovery & Prognosis
Recovery from brachial neuritis varies greatly between individuals but in most cases people make a full, or nearly full recovery.
Usually, the pain settles within a few weeks, but it can take a number of months to regain full strength and range of motion at the shoulder after brachial neuritis. Around 80% of people who suffer from brachial plexopathy will make a full recovery within 2 years, with another 10% recovering further in the following year.
In some cases, people will be left with persistent pain and/or weakness and reduced endurance in the shoulder muscles. Recovery time is often linked to how long the painful phase lasts i.e. longer painful phase = longer recovery time.
Recovery from parsonage turner syndrome tends to take longer if symptoms are bilateral (in both arms). Recurrence is more common with inherited brachial neuritis (approximately 75% recurrence rate) than idiopathic brachial plexopathy (between 5-26% recurrence).
What Else Can Help?
Shoulder and arm exercises are key to making a full recovery from Parsonage Turner Syndrome once the pain is under control:
- Shoulder Mobility Exercises: can be done in the early stages
- Rotator Cuff Strengthening: first step to regaining strength
- Scapular Stability Exercises: regain scapular control
- Shoulder Rehab Exercises: final stage of rehab
Aim to do your exercises around 30-60 minutes after taking any pain relief so that the effects have kicked in to get the best results and it's often best to avoid doing exercises just before you go to bed.
Brachial neuritis is just one possible cause of nerve pain in the arm and hand. Nerve pain can be the result of compression or irritation at the neck or anywhere down the path of the nerve and typically presents with pain, tingling, numbess and weakness on one arm - visit the arm nerve pain section to find out more.
If brachial neuritis isn't like the cause of your shoulder pain, check out the shoulder pain diagnosis section for help working out what is wrong.
Related Articles
Page Last Updated: December 10th, 2025
Next Review Due: December 10th, 2027