- Home
- Common Shoulder Problems
- Impingement Syndrome
Shoulder Impingement Syndrome
Written By: Chloe Wilson BSc (Hons) Physiotherapy
Reviewed By: SPE Medical Review Board
Shoulder impingement syndrome develops when the shoulder tendons get intermittently trapped and squashed underneath one of the shoulder bones, the acromion.
This impingement damages the soft tissues around the shoulder and can lead to pain, inflammation and reduced shoulder range of motion, particularly with activities when the arm is above the head.
Most commonly, shoulder impingement syndrome develops gradually over time through wear and tear on the shoulder, but it does sometimes develop following an injury. Impingement syndrome affects the rotator cuff muscles, the four main muscles that control the movement and stability of the shoulder.
Here, we will look at the common causes and symptoms of rotator cuff impingement, how it is diagnosed and the best treatment options for shoulder impingement syndrome to decrease pain and improve movement and strength.
What Is Shoulder Impingement?
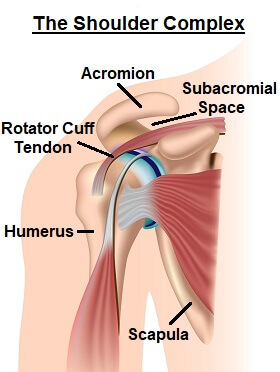
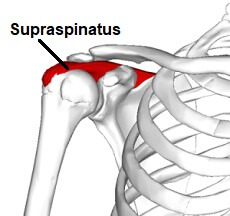
Shoulder impingement syndrome occurs at the top of the shoulder. The shoulder is made up of three bones:
- Humerus: upper arm bone
- Scapula: shoulder blade
- Clavicle: collar bone
The shoulder bones are connected together by ligaments, and one of them is the coacoacromial ligament, which connects the acromion and the coracoid process, bony projections off the scapula.
The acromion and the coracoacromial ligament form a sort of bridge or roof over the top of the shoulder known as the coracoacromial arch. The space underneath this arch is known as the subacromial space.
Each of the rotator cuff muscle tendons run through the subacromial space and as the arm moves up and down, the rotator cuff tendons slide backwards and forwards through this space.
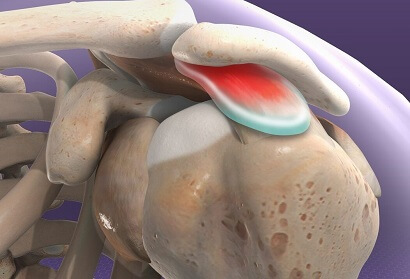
Sitting between the subacromial space and the rotator cuff tendons is the subacromial bursa, a small fluid filled sac that protects the tendons and prevents friction against the bone.
The space underneath the acromion is fairly small, and the gap gets narrower as you lift your arm up because of how the bones and tendons move.
Shoulder impingement syndrome refers to a number of problems that can develop in this area, the common characteristic being that the subacromial space narrows more than usual leading to pinching or friction on the soft tissues.
Causes of Shoulder Impingement Syndrome
Shoulder impingement syndrome commonly affects people who engage in activities requiring repetitive overhead arm movements or heavy lifting such as swimming, throwing, weightlifting and racket sports, or occupations such as building, decorating and electrical work. It is also often associated with aging.
The common causes of subacromial impingement fall into two categories:
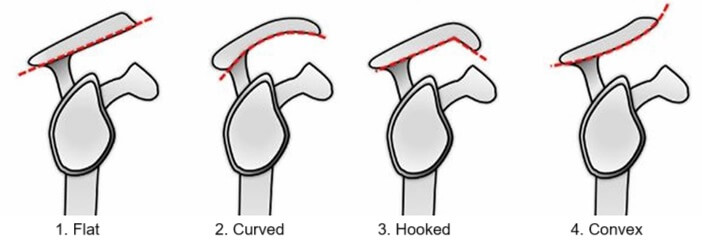
- Primary Shoulder Impingement: from bony abnormalities. Occurs when there are changes in the shape or angle of the acromion that reduce the size of the subacromial space from wear and tear or a congenital abnormality
- Secondary Shoulder Impingement: from dynamic instability. A combination of weakness and/or tightness in the shoulder muscles alters the position of the acromion, reducing the subacromial space. This leads to repetitive friction on the soft tissues which in turn causes inflammation.
Let's look at these different causes of shoulder impingement syndrome in some more detail.
1. Degeneration
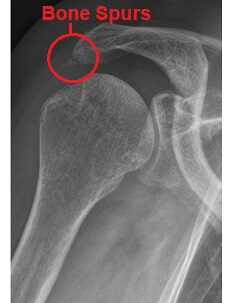
A common cause of primary shoulder impingement syndrome is wear and tear of the acromion which results in bone spurs.
Rather than the acromion being smooth, small outgrowths of bone stick out and rub on the rotator cuff tendons, leading to shoulder impingement syndrome.
This degeneration may happen through repetitive movements or as part of the normal aging process.
2. Congenital Abnormalities
Another common cause of primary shoulder impingement syndrome is a congenital abnormality - i.e. present since birth. I
n some people, the acromion forms at a slightly different angle affecting the shape of the acromial arch which can reduce the space in the subacromial space. This also increases the friction on the rotator cuff tendons leading to shoulder impingement syndrome.
3. Shoulder Tendonitis
One of the most common causes of secondary shoulder impingement syndrome is tendonitis, where repetitive friction on the rotator cuff and biceps tendons causes inflammation. This swelling reduces the subacromial space and as pressure builds up on the tendon, it reduces the blood flow causing further damage.
The rotator cuff tendons most commonly affected bu subacromial impingement are supraspinatus and long head of biceps as they runs directly through the subacromial space. Inflammation in these tendons is known as supraspinatus tendonitis aka painful arc syndrome and biceps tendonitis.
Tendonitis can occur from a one-off injury, repetitive movements or overuse. In some cases, calcium deposits can build up in the tendon. If left untreated, the tendon may even tear – see the rotator cuff tear section for more information.
4. Shoulder Bursitis
Another common cause of secondary shoulder impingement syndrome is bursitis. Excessive friction on the subacromial bursa leads to inflammation of the small fluid-filled sac, known as subacromial bursitis. Again, this reduces the subacromial space leading to shoulder impingement syndrome. You can find out more in the shoulder bursitis section.
Shoulder Impingement Symptoms
Symptoms start off fairly mild but get gradually worse as the condition progresses. Common symptoms of rotator cuff impingement include:
- Shoulder Pain: across the shoulder and sometimes extending down to the elbow. People often describe impingement like a toothache or a sharp pain. To start with, it will only be painful during activities but as the impingement syndrome progresses, you may develop pain even when resting.
Shoulder impingement syndrome pain tends to be worst when the arm is behind the back, e.g. fastening a bra, or above the head e.g. reaching into high cupboards or hanging up washing
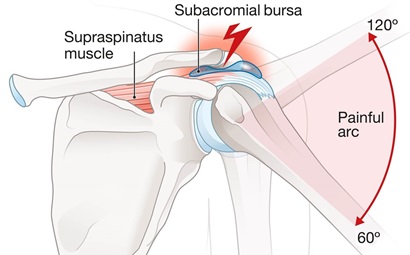
- Painful Arc: Movements below shoulder height tend not to be painful with shoulder impingement syndrome, but as you raise the arm up above shoulder height, pain often develops.
Depending on the cause of the impingement, the pain may actually decrease again once the arm is up straight due to the change in position of the bones in the shoulder which opens up the subacromial space.
In these cases, the most painful part of the movement tends to be from around 70 degrees abduction up to 120 degrees, known as a painful arc. This is a classic feature of supraspinatus tendonitis - Weakness: the shoulder muscles may start to weaken. This tends to be most noticeable with overhead activities
- Difficulty Sleeping: It may become painful to lie on the affected shoulder with impingement syndrome
- Problems with Lifting: Lifting heavy objects, especially overhead may become difficult and painful
- Loss of Movement: shoulder motion may become restricted but this tends to develop later rather than when you first develop shoulder impingement syndrome
Diagnosing Rotator Cuff Impingement
Your doctor can usually diagnosis shoulder impingement syndrome from your history and for examining you. They will look for the presence of a painful arc, or increased pain with movements overhead and will test the strength of your shoulder muscles.
They may also carry out special tests to confirm shoulder impingement syndrome such as the Empty Can test or Hawkins Kennedy test. You can try simple versions of these shoulder impingement tests at home.
In some cases, your doctor may send you for further tests if they suspect shoulder impingement syndrome. X-rays may be done to check for the presence of bone spurs and to rule out other conditions. An ultrasound scan may be done to assess the soft tissues for any damage such as bursitis, rotator cuff tears or calcium deposits in the tendon.
Shoulder Impingement Treatment
Successful treatment of shoulder impingement syndrome relies on correctly identifying the cause of the impingement e.g. you would treat impingement from bone spurs differently from impingement due to muscle imbalance. Without this, treatment will be ineffective and even if the pain does settle, it is likely to return.
Most cases of shoulder impingement syndrome can be treated conservatively, but in some cases, particularly if the bone is affected, surgery may be required.
#CommissionsEarned from Amazon on qualifying purchases
Non-Surgical Treatment
Treatment for shoulder impingement syndrome aims to reduce pain and inflammation, and restore motion and strength and may consist of:

- Exercises: Strengthening, stretching and stability exercises for shoulder impingement syndrome are the best place to start. They help to open up the subacromial space and take the pressure and friction off the irritated tendons.
- Rest: avoiding activities that aggravate your symptoms for a period, such as any movements placing your arm above your head or behind your back, is really important to allow the inflammation to settle
- Medication: anti-inflammatory medication such as ibuprofen/Advil helps to reduce swelling and pain
- Cold Therapy: using an ice-pack regularly can help reduce pain and inflammation. Ice packs should be wrapped in a towel (unless they have a special cover) and placed over the shoulder for ten minutes, three to four times daily. You can get specially designed shoulder ice packs that attach around the shoulder joint to help it stay in place so that you can move around. For more information on how ice therapy works, see the ice therapy section on our sister site
- Physical Therapy: a physical therapist will first assess your shoulder to identify any areas of weakness, tightness, stiffness and instability that have caused the shoulder impingement syndrome and work on a rehab program with you. They may also do some manual therapy to restore motion and positioning at the shoulder, and ultrasound to reduce inflammation
- Improve Posture: Thinking about your posture, especially if you spend long periods on a computer or smart phone can make a big difference by reducing the pressure and friction through the soft tissues in and around the shoulder. There are some really simple things you can do to improve posture that can make a big difference
- Injections: corticosteroid injections can help to reduce inflammation in the tendons or bursa. A mixture of steroid and local anesthetic is injected into the area. Care needs to be taken initially as the injection temporarily weakens the tendon increasing the risk of rupture.
Injections should not be used as a stand-alone treatment, they should be followed by a course of physical therapy to ensure the problem doesn’t return. You can find out more about steroid injections on our sister site.
Surgery For Impingement Syndrome
In some cases of shoulder impingement syndrome, such as if there are bony spurs or if other treatment has failed, subacromial decompression surgery will be advised. Surgery aims to enlarge the subacromial space to make more space for the rotator cuff tendons.
Subacromial decompression surgery for shoulder impingement syndrome is usually carried out arthroscopically, aka keyhole surgery. Two or three small holes are made around the shoulder. A camera is inserted to allow the surgeon to see the structures via a video screen and small surgical instruments are inserted into the joint.
In most cases the surgeon will remove part of the acromion bone and sometimes part of the subacromial bursa. This is known as a subacromial decompression or acromioplasty. If they find any other issues such as arthritis or a rotator cuff tear, they will address those as well.
After surgery, you may be given a sling to wear initially. You will work with a physical therapist on a rehab program to regain full strength, motion and stability in the shoulder - visit the rotator cuff exercises section to find out more. It usually takes around 3-5 months to recover from shoulder impingement surgery.
Find out what happens during surgery and all about the rehab and recovery process in the subacromial decompression section.
What Else Can Help?
Shoulder impingement syndrome is one of the most common causes of shoulder and upper arm pain, and is often present alongside other shoulder problems such as bursitis and rotator cuff tears.
One of the best ways to reduce pain and inflammation and restore normal movement is shoulder impingement exercises, particularly focusing on scapula stability exercises initially. Improving your posture, particularly when sitting at your desk can also really help.
There are also a number of other possible causes of shoulder pain. If shoulder impingement syndrome is not sounding like your problem, visit the shoulder injuries guide or check out our shoulder pain diagnosis charts.
Related Articles
Shoulder Problems
November 6th, 2024
Diagnose Your Pain
May 8th, 2024
Rehab Exercises
December 12, 2023
Page Last Updated: April 29th, 2025
Next Review Due: April 29th, 2027