- Home
- Wrist Pain Diagnosis
- Wrist Fractures
- Smith Fracture
Smith's Fracture Wrist
Written By: Chloe Wilson BSc (Hons) Physiotherapy
Reviewed By: SPE Medical Review Board

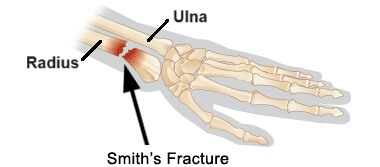
A Smith’s fracture is a type of wrist fracture where the outer forearm bone breaks.
Typically caused by a fall on a bent wrist or a blow to the back of the hand, the distal radius bone in the forearm breaks and shifts forwards.
Distal radius fractures cause pain, swelling and often an obvious deformity at the wrist joint which can impact movement and function.
Once the broken fragments of the radius bone are realigned, with or without surgery, a cast is worn for a few weeks to allow the fracture to heal in the correct position.
Here we will look at the common causes and symptoms of a Smith’s fracture, how it varies from other wrist fractures such as colles vs smith fracture, the diagnosis process and the best treatment options, including when surgery is necessary.
What Is A Smith Fracture?
A Smith’s fracture is a break in the distal radius, near the wrist joint.
The forearm is made up of two long bones that run between the elbow and the wrist:
- Radius: found on the thumb side of the forearm
- Ulna: found on the pinky side of the forearm
Wrist fractures of the radius and/or ulna are a common injury and there are a number of different types depending on where the break occurs, the direction of the break and where the broken bone shifts to.
With a Smith’s Fracture:
- Location: the break occurs in the lower (distal) end of the radius bone near the wrist
- Displacement: the broken fragment of the radius shifts towards the palm side of the wrist, known as volar displacement
Types Of Smith Fracture
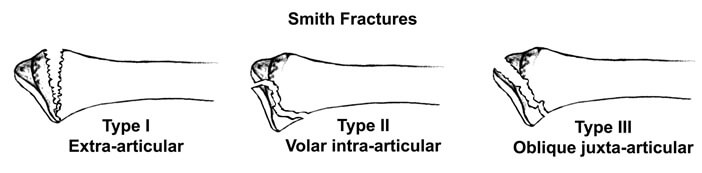
A Smith distal radius fracture can be classified into three types:
- Type 1 Smith’s Fracture: an extra articular transverse fracture of the distal radius. Extra-articular means it doesn’t extend into the wrist joint, and transverse means the break runs in a straight line across the bone, perpendicular its length. Most common type accounting for around 85% of Smith’s fractures
- Type 2 Smith’s Fracture: Intra-articular oblique fracture of the distal radius. Intra-articular means it extends into the wrist joint and oblique means the bone is broken at an angle. Accounts for around 13% of Smith’s fractures
- Type 3 Smith’s Fracture: a juxta-articular oblique fracture. Juxta-articular means the break is near the joint line but doesn’t actually extend into it. Accounts for only around 2% of Smith distal radius fractures
There are a few different types of distal radius fracture, the most common being a Colles Fracture.
Causes Of Smith’s Fracture
Common causes of a Smith’s Fracture wrist include:
- Fall: onto a flexed (bent wrist). Falling onto the hand when the wrist is bent forwards means the force goes through the back of the hand rather than the palm, which pushes the distal radius forwards (volarly direction). A fall onto a flexed wrist is the most common cause of a Smith’s fracture and can occur during various activities such as walking on uneven surfaces, falling while cycling, slipping on ice or losing balance and falling
- Direct Trauma: Another common cause of a Smith’s fracture is a direct blow or impact to the back of the wrist/forearm (aka dorsal aspect). This can happen in scenarios such as contact sports (e.g. football, rugby), physical altercations, industrial injuries involving machinery or heavy objects, or accidents where the back of the forearm strikes a hard surface
- High-Impact Injuries: high-impact trauma, e.g. motor vehicle accidents or a fall from a significant height, can result in a Smith’s fracture wrist due to the substantial forces involved
- Osteoporosis: osteoporosis decreases bone density which weakens bones making them more susceptible to fractures from minor falls and trauma. With osteoporosis, even low-energy impacts, such as a simple fall from standing height can result in a fracture. Slips and trips are a common cause of Smith’s fractures in people with osteoporosis.
Smith’s fractures most commonly affect young males after high energy falls and elderly women with osteoporosis after a lower energy fall.
Colles Vs Smiths Fracture
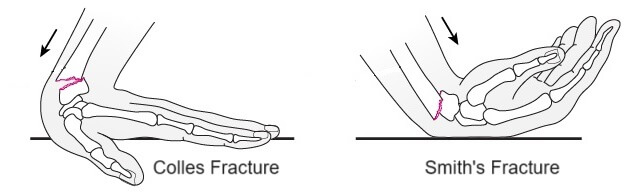
A Smith’s Fracture is also known as a Reverse Colles Fracture because while the location of the two types of break is very similar, the broken bone displaces in opposite ways.
- Colles Fractures: the broken piece of bone shifts backwards – towards the back of your hand, known as dorsal displacement. Typically caused by a fall onto an outstretched hand (wrist extended)
- Smith’s Fracture: the broken piece of bone shifts forwards – towards your palm, known as volar displacement. Typically caused by a fall onto a bent wrist.
Smith’s Fracture Symptoms
Common symptoms of a Smith’s fracture includes:
- Pain: immediate pain at the time of injury, usually localized to the distal forearm and wrist area. Pain from a Smith’s fracture is often sharp and gets worse with wrist movements or pressure over the affected area, particularly on the volar (palm) side of the wrist
- Swelling: significant swelling usually develops rapidly after injury around the wrist and distal forearm. There may also be bruising or discoloration around the injury site
- Deformity: a visible deformity, often described as a “garden spade” or “reverse dinner fork deformity” is common with a Smith fracture wrist due to the volar displacement of the distal radius
- Restricted Movement: wrist and forearm movement is often limited due to pain and structural disruption following a smith distal radius fracture
- Numbness & Tingling: if the Smith’s fracture affects nearby nerves there may be numbness or a pins and needles sensation in the hand. Up to 15% of Smith’s fractures show symptoms of acute carpal tunnel syndrome with medial nerve compression causing symptoms in a middle 3 fingers (palm side). Occasionally, there may be ulnar nerve compression causing symptoms in the front and back of the ring and little finger, or radial nerve compression causing symptoms in the front and back of the thumb and index finger
- Weakness: weakness in the wrist and reduced grip strength is common following a Smith’s fracture which can cause difficulty holding or manipulating objects and make it challenging to perform even light tasks such as writing, typing and cooking
Diagnosing Smith Fracture Wrist
Diagnosing a Smith's fracture involves several key steps to confirm the presence and extent of the fracture:
Medical History and Physical Examination
Following a wrist injury, your doctor will perform a:
- History: The healthcare provider will ask about the mechanism of injury, symptoms, and any previous wrist injuries.
- Examination: A thorough physical examination of the wrist and forearm is performed to assess swelling, deformity, tenderness, and range of motion.
Imaging Studies
If they suspect a Smith's fracture wrist, they may also send you for imaging studies:

- X-rays: The primary diagnostic tool, Smith fracture X-rays of the wrist and forearm are taken from multiple angles (anteroposterior, lateral, and oblique views) to visualize the fracture, assess the angle and displacement, and check for any additional fractures. You can see a classic Smith Fracture X-ray here.
- CT Scans: In cases of complex fractures or when detailed imaging is required, a CT scan provides a more comprehensive view of the bone fragments and surrounding structures.
- MRI: Occasionally used if there is concern about associated soft tissue injuries, such as ligament damage or nerve involvement.
Smith Fracture Treatment
Treatment for a Smith's fracture aims to realign the broken bone fragments, ensure proper healing, restore function, and prevent complications. The approach can be non-surgical or surgical, depending on the severity of the fracture and the degree of displacement.
Non-Surgical Treatment
Non-surgical treatment for a Smith's fracture may involve:
- Immobilization: For non-displaced or minimally displaced, stable Smith distal radius fractures, a cast or splint is applied to immobilize the wrist and forearm. This holds the bones in good alignment so that they heal in the correct position.
- Closed Reduction: If the fracture is displaced or unstable but can be realigned without surgery, a closed reduction is performed. This involves manipulating the bone fragments back into place manually with traction and may be done under local anaesthetic, sedatives or general anaesthetic. After realignment, a cast or splint is applied to maintain the position, usually holding the wrist in slight extension
The American Academy of Orthopedic Surgeons (AAOS) recommends weekly x-rays for the first three weeks after reduction and immobilization and before cast or splint removal to check that the fracture is healing in the right position.
Surgical Treatment
For more complex Smith's fractures, surgery may be required:
1. Open Reduction and Internal Fixation (ORIF)
For Smith fractures that are significantly displaced, unstable, or involve multiple bone fragments, ORIF is performed. This surgery involves making an incision to directly visualize and realign the bone fragments. The fragments are then secured in position with a metal plate and screws, or pins/K-wires.
A well-padded cast or sometimes a splint is then applied which is usually worn for 4-6 weeks. The sutures (stitches) are removed after 7-10 days and x-rays are taken to check the position. If K-wires were used they are usually removed after 6 weeks
2. External Fixation
In cases with severe soft tissue injury or when internal fixation is not suitable, an external fixator (a frame outside the body attached to the bone with pins) is used to stabilize the Smith distal radius fracture.
This is usually left in place for around 6 weeks, or longer if the fracture is particularly unstable or when healing is delayed.
Recovery
Recovery from a Smith’s fracture usually involves the following:
- Initial Phase (0-6 Weeks): The wrist is immobilized in a cast or splint whether you’ve needed surgery or not. Pain and swelling are managed with regular ice, elevation, and pain medication e.g. paracetamol/acetaminophen or ibuprofen/Advil. You will be given exercises to do every day for your shoulder, elbow and hand to make sure they don’t get weak or stiff. You will also have regular follow-up appointments to monitor the healing process and ensure the fracture is stable.
- Intermediate Phase (6-12 Weeks): The cast or splint is typically removed after around 6 weeks. As soon as the cast has been removed you will start physical therapy, concentrating on gentle range-of-motion exercises to restore wrist flexibility and prevent stiffness. Gradual strengthening exercises are then introduced as healing progresses.
- Advanced Phase (3-6 Months): Physical therapy will now focus on strengthening, coordination, and functional activities to restore full wrist and hand function. You will gradually be able to return to normal activities, with restrictions on heavy lifting or high-impact activities until complete healing is confirmed.
- Long-Term Recovery (6+ Months): Complete recovery following a Smith’s fracture, including the ability to perform all activities without pain or limitation, typically occurs within 3-6 months. Some cases may take longer, especially if there were complications or additional injuries.
It is really important to follow your rehab plan throughout the recovery process to ensure you regain full range of motion, strength and function following a Smith’s fracture wrist.
Complications and Management
Most people make a good recovery after a Smith’s fracture but there are possible ongoing problems that some may experience:
- Nonunion or Malunion: Failure of the bone to heal properly, requiring additional treatment or surgery. Malunion can cause residual displacement or shortening of the distal radius resulting in a cosmetic abnormality referred to as a “garden spade deformity”
- Stiffness and Reduced Mobility: Persistent stiffness may require prolonged physical therapy or, in severe cases, surgical intervention
- Persistent Pain: Some people have problems with ongoing pain and chronic regional pain syndrome (CRPS) particularly with complex Smith’s fractures with associated tissue damage
- Post-Traumatic Arthritis: Development of arthritis in the wrist joint due to the Smith’s fracture
- Nerve or Tendon Damage: Injury to surrounding nerves or tendons, leading to numbness, weakness, or reduced function, may need specialized treatment.
Smith's Fracture Summary
A Smith’s fracture is a type of distal radius fracture at the wrist.
The classic feature of a Smith’s fracture is volar displacement of the radius, where the bone shifts towards the palm side of the wrist, known as a reverse dinner plate deformity.
Smith distal radius fractures typically result from falls onto a flexed wrist, direct trauma to the dorsal (back) forearm, high-impact injuries, osteoporosis-related falls, and industrial or workplace accidents.
Symptoms include pain, swelling, bruising, garden spade deformity, weakness and restricted movement.
Often, a Smith fracture can be treated without the need for surgery with a closed reduction and cast, but in some cases surgery may be required to stabilize the bone.
A cast is worn for around 6 weeks following a Smith fracture wrist and then treatment focuses on regaining strength and function with rehab exercises.
There are lots of different types of distal radius fracture such as Colles fractures and Barton fractures, and they are often associated with wrist fractures too, such as an ulna styloid fracture.
Alternatively, visit the radial wrist pain or wrist pain diagnosis chart section for help working out what is causing your wrist pain.
Related Articles
Medical & Scientific References
- Smith Fracture Review. National Library Of Medicine. January 2024
- Smith Fracture. Radiopaedia. June 2023
- Smith Fracture. Science Direct
Page Last Updated: February 22nd, 2025
Next Review Due: February 22nd, 2027